Dabigatran Etexilate Mesylate
Indications
Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation: Dabigatran Etexilate Mesylate is indicated to reduce the risk of stroke and systemic embolism in patients with non-valvular atrial fibrillation.
Treatment of Deep Venous Thrombosis and Pulmonary Embolism: Dabigatran Etexilate Mesylate is indicated for the treatment of deep venous thrombosis and pulmonary embolism in patients who have been treated with a parenteral anticoagulant for 5-10 days.
Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism: Dabigatran Etexilate Mesylate is indicated to reduce the risk of recurrence of deep venous thrombosis and pulmonary embolism in patients who have been previously treated.
Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism Following Hip Replacement Surgery: Dabigatran Etexilate Mesylate is indicated for the prophylaxis of deep vein thrombosis and pulmonary embolism, in patients who have undergone hip replacement surgery.
Treatment of Deep Venous Thrombosis and Pulmonary Embolism: Dabigatran Etexilate Mesylate is indicated for the treatment of deep venous thrombosis and pulmonary embolism in patients who have been treated with a parenteral anticoagulant for 5-10 days.
Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism: Dabigatran Etexilate Mesylate is indicated to reduce the risk of recurrence of deep venous thrombosis and pulmonary embolism in patients who have been previously treated.
Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism Following Hip Replacement Surgery: Dabigatran Etexilate Mesylate is indicated for the prophylaxis of deep vein thrombosis and pulmonary embolism, in patients who have undergone hip replacement surgery.
Pharmacology
Dabigatran and its acyl glucuronides are competitive, direct thrombin inhibitors. Because thrombin (serine protease) enables the conversion of fibrinogen into fibrin during the coagulation cascade, its inhibition prevents the development of a thrombus. Both free and clot-bound thrombin, and thrombin-induced platelet aggregation are inhibited by the active moieties.
At recommended therapeutic doses, dabigatran etexilate prolongs the coagulation markers such as aPTT, ECT, and TT. INR is relatively insensitive to the exposure to dabigatran and cannot be interpreted the same way as used for warfarin monitoring. The aPTT test provides an approximation of Dabigatran Etexilate’s anticoagulant effect. The average time course for effects on aPTT, following approved dosing regimens in patients with various degrees of renal impairment is shown in Figure 2. The curves represent mean levels without confidence intervals; variations should be expected when measuring aPTT. While advice cannot be provided on the level of recovery of aPTT needed in any particular clinical setting, the curves can be used to estimate the time to get to a particular level of recovery, even when the time since the last dose of Dabigatran Etexilate is not precisely known. In the RE-LY trial, the median (10 th to 90 th percentile) trough aPTT in patients receiving the 150 mg dose was 52 (40 to 76) seconds.
At recommended therapeutic doses, dabigatran etexilate prolongs the coagulation markers such as aPTT, ECT, and TT. INR is relatively insensitive to the exposure to dabigatran and cannot be interpreted the same way as used for warfarin monitoring. The aPTT test provides an approximation of Dabigatran Etexilate’s anticoagulant effect. The average time course for effects on aPTT, following approved dosing regimens in patients with various degrees of renal impairment is shown in Figure 2. The curves represent mean levels without confidence intervals; variations should be expected when measuring aPTT. While advice cannot be provided on the level of recovery of aPTT needed in any particular clinical setting, the curves can be used to estimate the time to get to a particular level of recovery, even when the time since the last dose of Dabigatran Etexilate is not precisely known. In the RE-LY trial, the median (10 th to 90 th percentile) trough aPTT in patients receiving the 150 mg dose was 52 (40 to 76) seconds.
Dosage & Administration
Reduction in Risk of Stroke and Systemic Embolism in Non-valvular AF-
Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation: For patients with creatinine clearance (CrCl) >30 mL/min, the recommended dose of Dabigatran Etexilate is 150 mg taken orally, twice daily. For patients with severe renal impairment (CrCl 15-30 mL/min), the recommended dose of Dabigatran Etexilate is 75 mg twice daily. Dosing recommendations for patients with a CrCl <15 mL/min or on dialysis cannot be provided.
Treatment of Deep Venous Thrombosis and Pulmonary Embolism: For patients with CrCl >30 mL/min, the recommended dose of Dabigatran Etexilate is 150 mg taken orally, twice daily, after 5-10 days of parenteral anticoagulation. Dosing recommendations for patients with a CrCl ≤30 mL/min or on dialysis cannot be provided.
Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism: For patients with CrCl >30 mL/min, the recommended dose of Dabigatran Etexilate is 150 mg taken orally, twice daily after previous treatment. Dosing recommendations for patients with a CrCl ≤30 mL/min or on dialysis cannot be provided.
Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism Following Hip Replacement Surgery: For patients with CrCl >30 mL/min, the recommended dose of Dabigatran Etexilate is 110 mg taken orally 1-4 hours after surgery and after hemostasis has been achieved, then 220 mg taken once daily for 28-35 days. If Dabigatran Etexilate is not started on the day of surgery, after hemostasis has been achieved initiate treatment with 220 mg once daily. Dosing recommendations for patients with a CrCl ≤30 mL/min or on dialysis cannot be provided
- CrCl >30 mL/min: 150 mg twice daily
- CrCl 15 to 30 mL/min: 75 mg twice daily
- CrCl <15 mL/min or on dialysis: Dosing recommendations cannot be provided
- CrCl 30 to 50 mL/min with concomitant use of P-gp inhibitors: Reduce dose to 75 mg twice daily if given with P-gp inhibitors dronedarone or systemic ketoconazole.
- CrCl <30 mL/min with concomitant use of P-gp inhibitors: Avoid co-administration
- CrCl >30 mL/min: 150 mg twice daily
- CrCl ≤30 mL/min or on dialysis: Dosing recommendations cannot be provided
- CrCl <50 mL/min with concomitant use of P-gp inhibitors: Avoid co-administration
- CrCl >30 mL/min: 110 mg for first day, then 220 mg once daily
- CrCl ≤30 mL/min or on dialysis: Dosing recommendations cannot be provided
- CrCl <50 mL/min with concomitant use of P-gp inhibitors: Avoid co-administration.
Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation: For patients with creatinine clearance (CrCl) >30 mL/min, the recommended dose of Dabigatran Etexilate is 150 mg taken orally, twice daily. For patients with severe renal impairment (CrCl 15-30 mL/min), the recommended dose of Dabigatran Etexilate is 75 mg twice daily. Dosing recommendations for patients with a CrCl <15 mL/min or on dialysis cannot be provided.
Treatment of Deep Venous Thrombosis and Pulmonary Embolism: For patients with CrCl >30 mL/min, the recommended dose of Dabigatran Etexilate is 150 mg taken orally, twice daily, after 5-10 days of parenteral anticoagulation. Dosing recommendations for patients with a CrCl ≤30 mL/min or on dialysis cannot be provided.
Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism: For patients with CrCl >30 mL/min, the recommended dose of Dabigatran Etexilate is 150 mg taken orally, twice daily after previous treatment. Dosing recommendations for patients with a CrCl ≤30 mL/min or on dialysis cannot be provided.
Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism Following Hip Replacement Surgery: For patients with CrCl >30 mL/min, the recommended dose of Dabigatran Etexilate is 110 mg taken orally 1-4 hours after surgery and after hemostasis has been achieved, then 220 mg taken once daily for 28-35 days. If Dabigatran Etexilate is not started on the day of surgery, after hemostasis has been achieved initiate treatment with 220 mg once daily. Dosing recommendations for patients with a CrCl ≤30 mL/min or on dialysis cannot be provided
Interaction
Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation: The concomitant use of Dabigatran Etexilate with P-gp inducers (e.g., rifampin) reduces exposure to dabigatran and should generally be avoided. P-gp inhibition and impaired renal function are the major independent factors that result in increased exposure to dabigatran. Concomitant use of P-gp inhibitors in patients with renal impairment is expected to produce increased exposure of dabigatran compared to that seen with either factor alone. In patients with moderate renal impairment (CrCl 30-50 mL/min), reduce the dose of Dabigatran Etexilate to 75 mg twice daily when administered concomitantly with the P-gp inhibitors dronedarone or systemic ketoconazole. The use of the P-gp inhibitors verapamil, amiodarone, quinidine, clarithromycin, and ticagrelor does not require a dose adjustment of Dabigatran Etexilate. These results should not be extrapolated to other P-gp inhibitors. The concomitant use of Dabigatran Etexilate and P-gp inhibitors in patients with severe renal impairment (CrCl 15-30 mL/min) should be avoided.
Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism: Avoid use of Dabigatran Etexilate and P-gp inhibitors in patients with CrCl <50 mL/min.
Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism Following Hip Replacement Surgery: In patients with CrCl ≥50 mL/min who have concomitant administration of P-gp inhibitors such as dronedarone or systemic ketoconazole, it may be helpful to separate the timing of administration of dabigatran and the P-gp inhibitor by several hours. The concomitant use of Dabigatran Etexilate and P-gp inhibitors in patients with CrCl <50 mL/min should be avoided.
Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism: Avoid use of Dabigatran Etexilate and P-gp inhibitors in patients with CrCl <50 mL/min.
Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism Following Hip Replacement Surgery: In patients with CrCl ≥50 mL/min who have concomitant administration of P-gp inhibitors such as dronedarone or systemic ketoconazole, it may be helpful to separate the timing of administration of dabigatran and the P-gp inhibitor by several hours. The concomitant use of Dabigatran Etexilate and P-gp inhibitors in patients with CrCl <50 mL/min should be avoided.
Contraindications
Dabigatran Etexilate is contraindicated in patients with:
- Active pathological bleeding.
- History of a serious hypersensitivity reaction to Dabigatran Etexilate (e.g., anaphylactic reaction or anaphylactic shock).
- Mechanical prosthetic heart valve.
Side Effects
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Increased Risk of Thrombotic Events after Premature Discontinuation
- Risk of Bleeding
- Spinal/Epidural Anesthesia or Puncture
- Thromboembolic and Bleeding Events in Patients with Prosthetic Heart Valves
- Increased Risk of Thrombosis in Patients with Triple-Positive Antiphospholipid Syndrome
Pregnancy & Lactation
Pregnancy: The limited available data on Dabigatran Etexilate use in pregnant women are insufficient to determine drug-associated risks for adverse developmental outcomes. There are risks to the mother associated with untreated venous thromboembolism in pregnancy and a risk of hemorrhage in the mother and fetus associated with the use of anticoagulant
Lactation: There are no data on the presence of dabigatran in human milk, the effects on the breastfed child, or on milk production. Dabigatran and/or its metabolites were present in rat milk. Breastfeeding is not recommended during treatment with Dabigatran Etexilate.
Lactation: There are no data on the presence of dabigatran in human milk, the effects on the breastfed child, or on milk production. Dabigatran and/or its metabolites were present in rat milk. Breastfeeding is not recommended during treatment with Dabigatran Etexilate.
Precautions & Warnings
Bleeding: Dabigatran Etexilate can cause serious and fatal bleeding
Bioprosthetic heart valves: Dabigatran Etexilate use not recommended
Increased Risk of Thrombosis in Patients with Triple-Positive Antiphospholipid Syndrome: Dabigatran Etexilate use not recommended
Bioprosthetic heart valves: Dabigatran Etexilate use not recommended
Increased Risk of Thrombosis in Patients with Triple-Positive Antiphospholipid Syndrome: Dabigatran Etexilate use not recommended
Use in Special Populations
Pediatric Use: The safety and effectiveness of Dabigatran Etexilate in pediatric patients have not been established.
Geriatric Use: Of the total number of patients in the RE-LY study, 82% were 65 and over, while 40% were 75 and over. The risk of stroke and bleeding increases with age, but the risk-benefit profile is favorable in all age groups.
Geriatric Use: Of the total number of patients in the RE-LY study, 82% were 65 and over, while 40% were 75 and over. The risk of stroke and bleeding increases with age, but the risk-benefit profile is favorable in all age groups.
Overdose Effects
Accidental overdose may lead to hemorrhagic complications. In the event of hemorrhagic complications, initiate appropriate clinical support, discontinue treatment with Dabigatran Etexilate, and investigate the source of bleeding. A specific reversal agent (idarucizumab) is available. Dabigatran is primarily eliminated by the kidneys with a low plasma protein binding of approximately 35%. Hemodialysis can remove dabigatran; however, data supporting this approach are limited. Using a high-flux dialyzer, blood flow rate of 200 mL/min, and dialysate flow rate of 700 mL/min, approximately 49% of total dabigatran can be cleared from plasma over 4 hours. At the same dialysate flow rate, approximately 57% can be cleared using a dialyzer blood flow rate of 300 mL/min, with no appreciable increase in clearance observed at higher blood flow rates. Upon cessation of hemodialysis, a redistribution effect of approximately 7% to 15% is seen. The effect of dialysis on dabigatran’s plasma concentration would be expected to vary based on patient specific characteristics. Measurement of aPTT or ECT may help guide therapy
Therapeutic Class
Anti-coagulants, Anti-platelet drugs, Fibrinolytics (Thrombolytics)
Storage Conditions
Store Dabigatran Etexilate at room temperature 20°C to 25°C. After opening the bottle, use Dabigatran Etexilate within 4 months. Safely throw away any unused Dabigatran Etexilate after 4 months. Keep Dabigatran Etexilate in the original bottle or blister package to keep it dry (protect the capsules from moisture). Do not put Dabigatran Etexilate in pill boxes or pill organizers. Tightly close your bottle of Dabigatran Etexilate right away after you take your dose. Keep Dabigatran Etexilate and all medicines out of the reach of children.
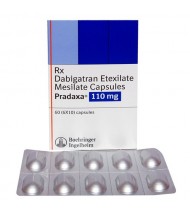
Capsule Pradaxa Capsule 110 mg
IndicationsReduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation: Da..
95.00Tk.
Pradaxa Capsule 150 mg
IndicationsReduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation: Da..
95.00Tk.
Showing 1 to 2 of 2 (1 Pages)